Consolidation with second high dose therapy and autologous stem cell transplantation is associated with improved overall survival in patients with multiple myeloma in first relapse
High dose chemotherapy and autologous stem cell transplantation (HDT/ASCT) remains the preferred first line consolidation strategy for fit patients with newly diagnosed multiple myeloma (MM). In the evolving era of new treatment options in second line, often including anti-CD38 antibodies, the role of HDT/ASCT is uncertain. This study evaluates real-world outcomes of MM patients in first relapse, specifically focusing on the role of consolidative HDT/ASCT.
We conducted a retrospective cohort study at the University Medical Centre Groningen, including MM patients who received first-line HDT/ASCT between 2008 and 2021. Patients were selected if they experienced a first relapse after a disease-free interval of at least 24 months with or 18 months without maintenance treatment. We evaluated the effectiveness of second-line treatment, in terms of time to next treatment or death (TTNT-D 2) and overall survival (OS), while identifying prognostic factors. A landmark analysis was performed six months post re-induction treatment, including only patients with a partial response (PR) or better.
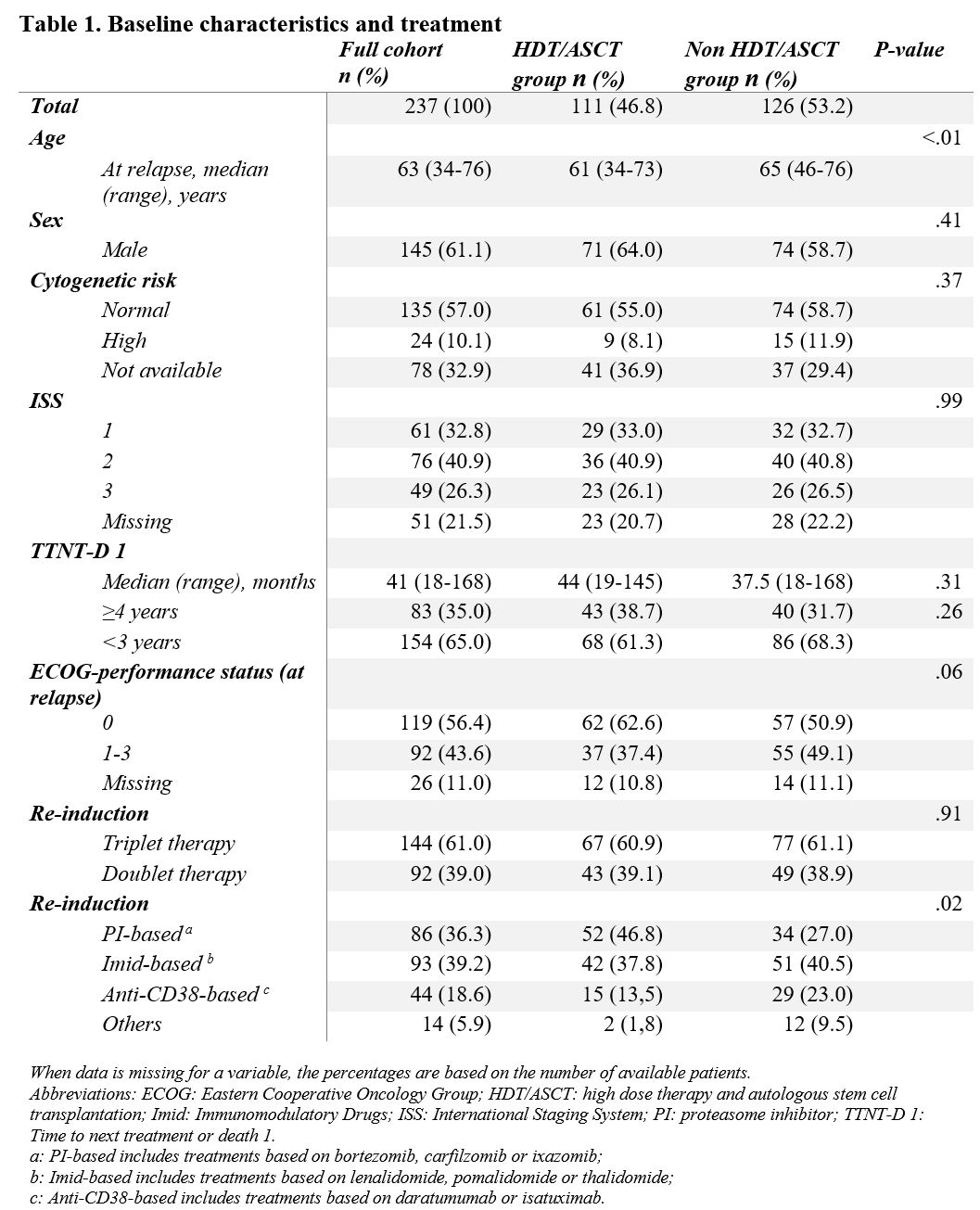
This study identified 237 patients with a first relapse potentially eligible for repeated HDT/ASCT. The median follow-up was 40 months. Second consolidative HDT/ASCT was applied in 111 patients (47%). Patients not treated with second HDT/ASCT were slightly older (65 vs. 61 years) and more frequently received anti-CD38 based re-induction (23% vs. 14%). HDT/ASCT was almost exclusively used in patients that achieved a PR or better after re-induction (Table 1).
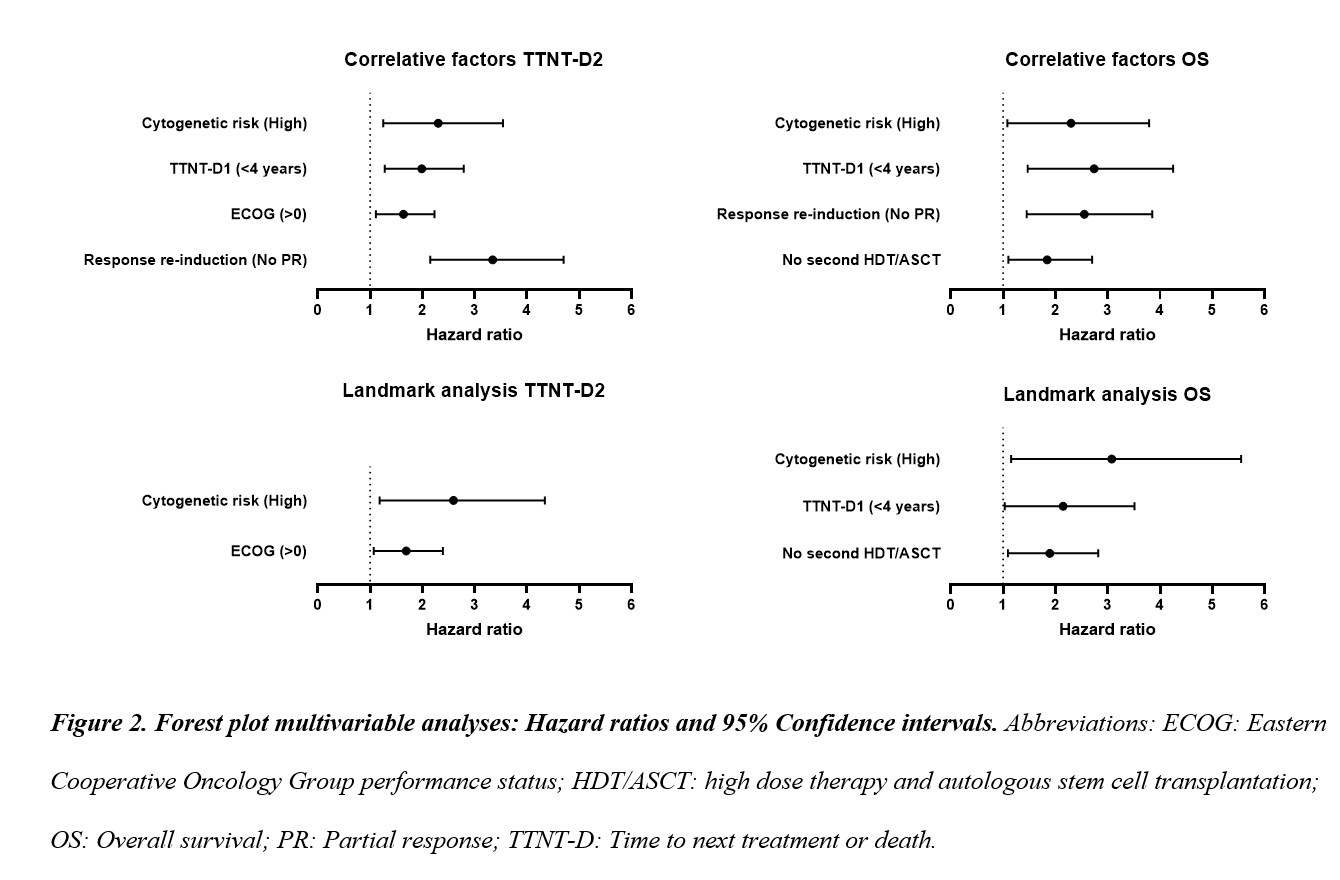
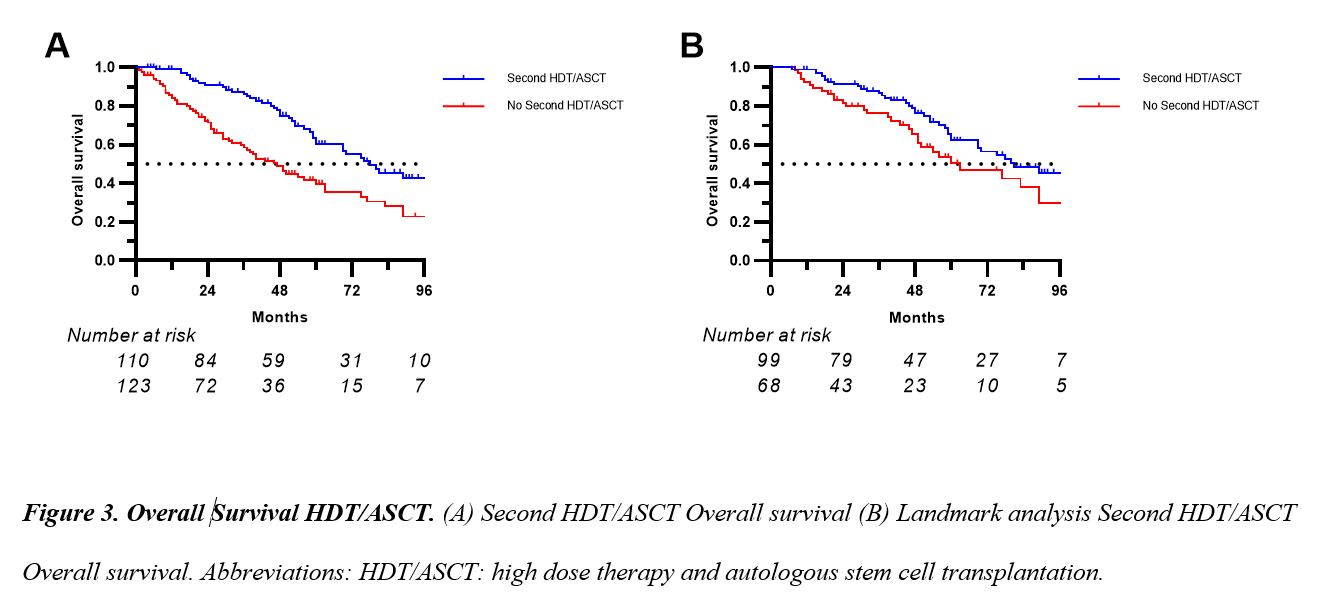
Multivariable analysis revealed that high-risk cytogenetics, shorter first response duration, poor performance status, and failure to achieve a PR were associated with shorter TTNT-D 2. All factors, but performance, were also associated with OS and the use of second HDT/ASCT emerged as additional positive prognostic factor. The landmark analysis confirmed that the use of second HDT/ASCT, along with absence of high-risk cytogenetics and a longer first response duration, was associated with a benefit in OS. (Figure 2,3) The transplantation-related mortality rate was <1%.
Our study demonstrated that second HDT/ASCT was mainly used in patients who achieved a PR or better. In the landmark analysis, second HDT/ASCT, alongside the absence of high-risk cytogenetics and a longer first response duration, was associated with improved OS. This study highlights the viability of second HDT/ASCT as treatment option for relapsed MM, especially after a durable response and limited toxicity with first HDT/ASCT. In the era of novel agents, second HDT/ASCT remains a valuable consolidative strategy, offering effective outcomes with limited additional toxicity. Given potential financial and quality of life benefits, further head-to-head research comparing second HDT/ASCT with novel therapies is warranted.