Prediction of 30-day readmission for vaso-occlusive crisis in patients with sickle cell disease
Sickle cell disease (SCD) is characterized by recurrent episodes of severe pain attacks, also called vaso-occlusive crisis (VOC), and are the most common reason for hospitalization. We previously were successful in developing machine learning models to predict pain using inpatient vital signs data as well as Apple Watch data in patients with SCD hospitalized for VOC. We now aimed to predict readmission within 30 days in patients with SCD treated for a VOC.
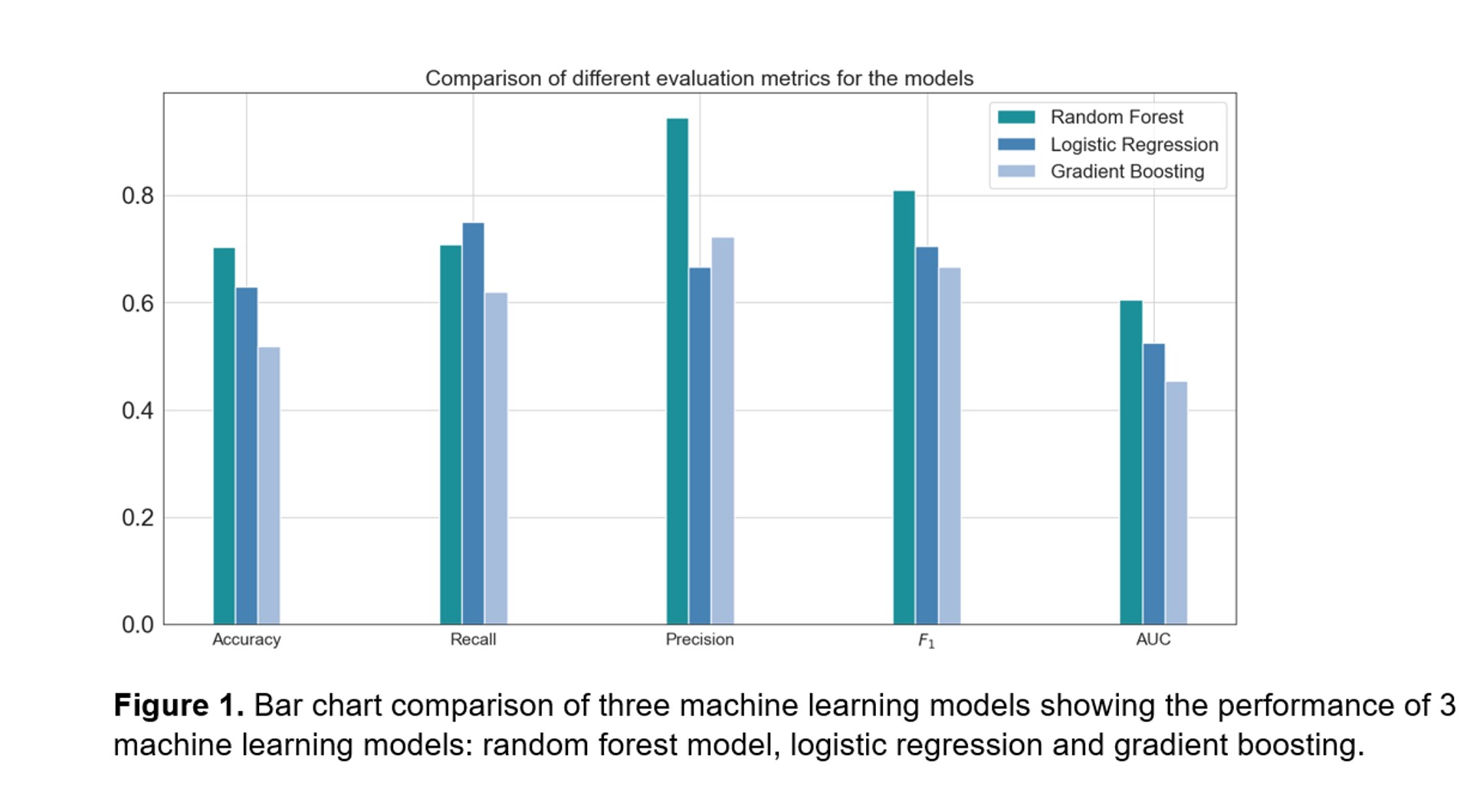
Patients with SCD aged 18 years and above, who were admitted for a VOC to the day hospital or Duke University Hospital between April and June 2022, were eligible for this study. Following informed consent, demographics, SCD genotype, details from the hospitalization such as length of stay, pain scores, as well as vital signs measured per standard of care were collected from the electronic medical records over 6 months before and 6 months after hospital admission. The vital signs over the entire hospital stay were averaged and those numbers were used as the predictor values for the model. The primary outcome was readmission defined as readmission within 30 days to the hospital hospital. The predictors were used to fit 3 different machine learning classification models for the prediction of readmission: random forest, logistic regression and gradient boosting. The performance of the machine learning models was evaluated using accuracy, precision, recall, F1 score and area under the receiver-operating-curve (AUC).
Eighteen participants with SCD were included in this study. The median age at inclusion was 30 years (IQR 22-34). The majority of the participants had SCD genotype HbSS (68%). There were 10 participants treated at the day hospital (56%), while the other 8 participants were admitted to the hospital with a median length of stay of 7.5 days (IQR 2.5-10). After discharge, 15 participants sought medical care at least once within 30 days (83%). This pilot study consisted of 88 vital sign data points across the 18 patients. The metrics of our best-performing machine learning model, the random forest model, were: accuracy 70%, precision 0.94, recall 0.71, F1 score 0.81 and AUC 0.61. To test how the model will perform for independent data sets, we used 5-fold cross-validation, and the cross-validation accuracy was 66% with a standard deviation of 7.7.
In this pilot study, our machine learning model was able to accurately predict readmission within 30 days following discharge, with real-time vital signs data collected during clinic visits and hospital admissions in participants with SCD.